2020 - A year in axSpA research! Part three
Good morning everyone!
I hope that you are having a lovely weekend.
Following on from last week, today’s blog post focuses on 4 additional publications from April – June, that didn’t quite fit with the themes covered last week (physical activity, smoking, obesity and biomarkers – https://www.projectnightingale.org/blogs/2020-a-year-in-axspa-research-part-two/).
As always, we hope you enjoy reading through the study overviews/ discussions. If you have any questions, or would like to talk through any of these studies in more detail, please feel free to get in touch by emailing our dedicated Project Nightingale researcher Rosie at rosie.barnett1@nhs.net and she will be happy to discuss with you (see September’s blog post for an introduction: https://www.projectnightingale.org/blogs/and-we-are-finally-back-with-the-regular-blog-posts/). If you are on twitter, you can also follow **https://twitter.com/RosieBarnett95 ** for regular research and Project Nightingale updates, including notifications for new blog posts!
If you yourself are interested in writing a blog post for us, we would also love to hear from you. Not only regarding your potential experiences with Project Nightingale, but also regarding your general experiences with axSpA. These can be posted anonymously, or with your name – whichever you prefer. Again, please email Rosie above, or get in touch using hello@projectnightingale.org. Here is a fantastic blog post published by John Wilkinson earlier this year, after receiving the challenge from his consultant: https://www.projectnightingale.org/blogs/john-wilkinson-no-holding-us-back/. Thank you so much for sharing your experiences John!
Thank you for reading and have a fabulous rest of the weekend everyone.
Best wishes,
The Project Nightingale Team
Characteristics associated with hospitalisation for COVID-19 in people with rheumatic disease: data from the COVID-19 Global Rheumatology Alliance physician-reported registry
May 2020. Gianfrancesco and colleagues. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7299648/
I am sure we are all more than tired of hearing the C-word! However, we understand that now is a particularly challenging and scary time for us all, perhaps especially if you have a chronic condition. And as such, feel it is important to present the aforementioned interesting study from the journal Annals of the Rheumatic Diseases, which has significantly contributed to the field of COVID research.
The present study included 600 individuals with rheumatic disease diagnosed with COVID, from 40 countries, as part of the COVID-19 Global Rheumatology Alliance registry. Encouragingly, over half the patients did not require hospitalisation. Treatment with biologics or traditional disease-modifying antirheumatic drugs (DMARDs) was associated with lower odds of hospitalisation, largely driven by anti-TNF therapies. While older age and presence of comorbidities such as hypertension, cardiovascular disease and diabetes were associated with increased risk of hospitalisation – as in the general population. Higher doses of prednisone (≥10 mg/day) were also associated with increased risk of hospitalisation. However, it is very important to note that due to the way in which case information was collected as part of the register, these rates should be interpreted with caution as are likely to be higher than people with rheumatic disease in the general population infected with COVID.
Interestingly, anti-TNF drugs such as adalimumab (Humira) and IL-6 inhibitors are now being trialled for potential treatment of COVID in the community, based on evidence from studies such as the one described above. While further evidence is absolutely needed in this area, it is exciting that some of this initial work indeed came from the field of Rheumatology!
See here for more information about the trialling of adalimumab for COVID-19: https://www.bmj.com/content/371/bmj.m3847 and here for more information about IL-6 inhibitors in COVID trials: https://inflammregen.biomedcentral.com/articles/10.1186/s41232-020-00134-7.

Do Illness Perceptions and Coping Strategies Change Over Time in Patients Recently Diagnosed With Axial Spondyloarthritis?
May 2020. Lunteren and colleagues. https://www.jrheum.org/content/early/2020/09/28/jrheum.191353.long
The present study by Lunteren and colleagues in the Netherlands explored change in illness perceptions and coping strategies over time in people recently diagnosed with axSpA. While back pain, disease activity, and health outcomes clearly improved over 2 years, illness perceptions and coping strategies remained remarkably stable. For example, at 2 years, people with axSpA still believed that their illness had severe “consequences” and they experienced negative emotions (e.g., feeling upset or fear) towards their illness, despite improvement in health outcomes. People most often coped with their pain by putting pain into perspective and tended to cope with limitations by being optimistic. Further research is recommended to explore why illness perceptions do not change despite improved outcomes, and to investigate the impact of these unchanged illness perceptions and coping strategies on health outcomes. Such research will be vital in order to understand how these negative perceptions can be improved.
How do you perceive your condition, and do you believe your perceptions to have changed over time? John Wilkinson recently wrote a post for our blog about his positive disposition and outlook in terms of his axSpA, even when hit with bad news: https://www.projectnightingale.org/blogs/john-wilkinson-no-holding-us-back/ - an excellent, empowering read. Thank you John! Again, please do get in touch if you would like to share your experiences – we would love to hear from you.
Biologic disease-modifying anti-rheumatic drugs and patient-reported outcomes in axial SpA: a systematic review and a call for action
June 2020. Rodrigues-Manica and colleagues. https://link.springer.com/article/10.1007%2Fs10067-020-05209-x
It is well recognised that therapeutic decisions should include both physicians and patients’ perspectives, since better outcomes are achieved through shared decision making. In this context, patient-reported outcomes (PROs) evaluation in axSpA has gained increasing importance in the clinical practice for therapeutic monitoring purposes. The present study aimed to assess the effectiveness of different biologic drugs based on PROs previously reported in the scientific literature through randomised controlled trials (RCTs – generally referred to as the “gold standard” for testing treatments).
While disease activity was most commonly reported as an outcome in RCTs, followed by function, both were very rarely reported using the “minimally clinically important difference” concept (an important concept used to determine whether a medical intervention improves perceived outcomes in people). The remaining PROs, concerning general and specific quality of life and fatigue, were less reported and in an even more varied way.
This review therefore highlights the fact that there is a need to raise the standard of care for axSpA, through the real introduction of the patient perspective in the decision-making process through inclusion of clearly defined, reported, and tested PROs and focussing more on these PRO-associated improvements in both clinical trials and importantly, clinical practice. In order to do this, the authors suggest there is a need to identify cut-offs for several PROs, equivalent to clinical remission (where there is a reduction or disappearance of the signs and symptoms of a disease), that should be addressed in the near future.
The figure below outlines a conceptual framework for PRO integration in clinical care taken from Dobrozsi and Panepint: https://doi.org/10.1182/asheducation-2015.1.501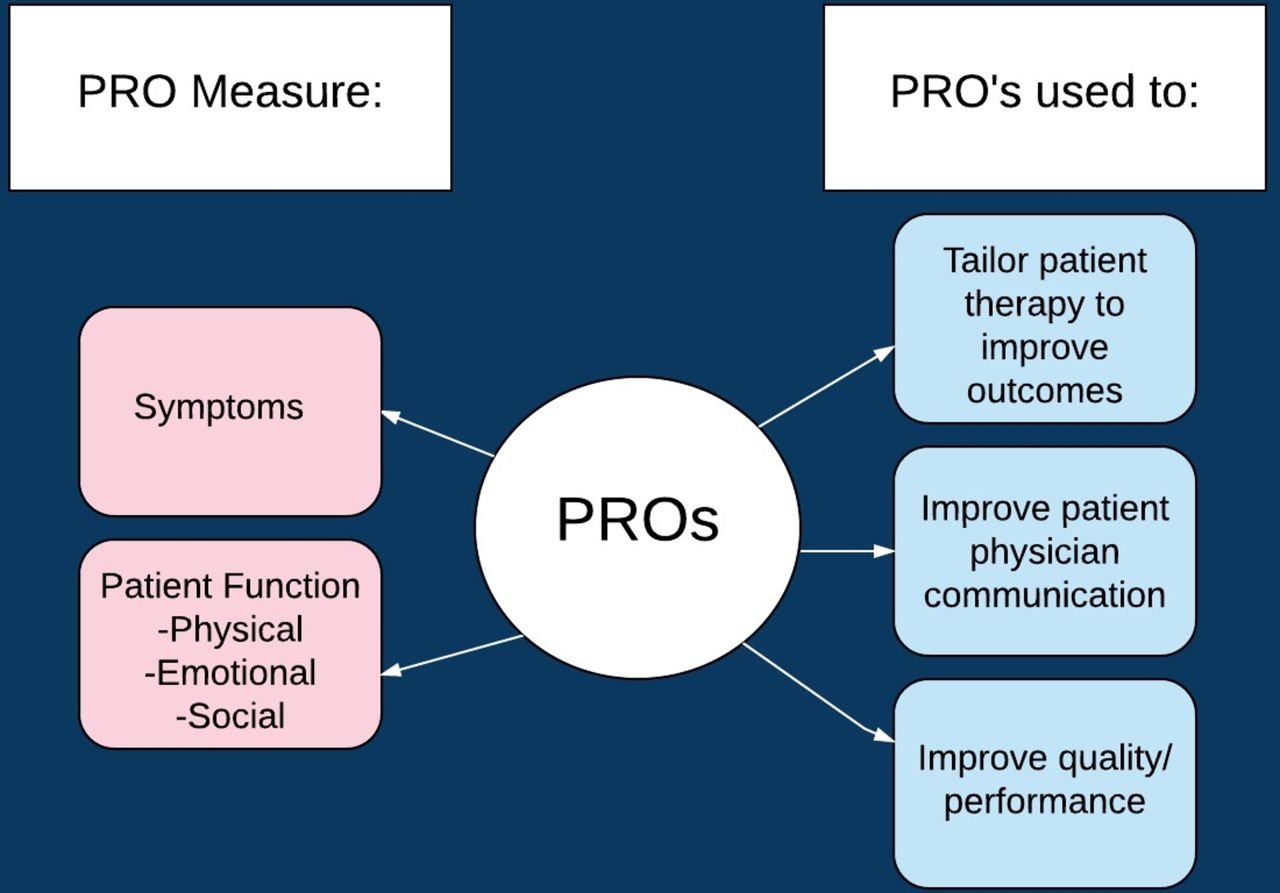
Machine learning–based prediction of radiographic progression in patients with axial spondyloarthritis
April 2020. Joo and colleagues. https://link.springer.com/article/10.1007%2Fs10067-019-04803-y
You may recognise this publication from our 2019 October axSpA research updates post, as this study was published online as a pre-print last year (https://www.projectnightingale.org/blogs/october-axspa-research-highlights/). This article used an exciting new statistical method of analyses known as machine learning – a bit of a buzzword in the research space at the moment! The authors developed statistical models driven by data from people with axSpA that could, with reasonable accuracy, predict radiographic progression. Further modelling with data from more people could provide an exciting opportunity for the clinical translation of such predictive models to highlight and improve the treatment of people who are at high-risk of progression. Very exciting work!