Understanding flare in axial spondyloarthritis: novel insights from daily self-reported flare experience
Hello everyone!
We hope that you are all having a good week! This week we have a bonus blog, as excitingly, our first full journal article utilising data from Project Nightingale has now been accepted for publication in Rheumatology Advances in Practice.
The publication provides new insights into axial spondyloarthritis (axSpA) flares, and was published online on the 15th November. To our knowledge, this is the first study to investigate, characterise and group daily self-reported flare profiles in people with axSpA, utilising a smartphone application and remote data collection. Below, we outline some of the key findings from the manuscript, and you can read the full publication online here. Thank you to all of our participants for your logging efforts! You can find out more about axSpA flares and how to manage them on the National Axial Spondyloarthritis Society website.
We also have an important Project Nightingale update published on our Home Page. If you are an active Project Nightingale user, you will be notified of this via the app in the coming days (if not already!). We will be publishing another blog tomorrow afternoon - the first in our "2021 - A year in axSpA research!" series.
If you have any questions, please do get in touch via email to hello@projectnightingale.org – we would love to hear from you.
Have a good rest of the week all!
Best Wishes,
The Project Nightingale Team
Key messages
- Daily self-reported smartphone data identified two distinct clusters of people living with axSpA who had different flare experiences.
- One group had a shorter, more intense flare experience (greater worsening of pain, mood, sleep, fatigue, stress).
- However, there were no differences in flare frequency between the groups.
- The group with prolonged flare had a significantly greater number of people who smoked.
- Despite differences in flare duration and symptoms, baseline clinical measures such as disease activity, function or spinal mobility, were similar between clusters.
- Smartphone technologies may therefore capture subtle changes in disease experience not currently considered in clinical practice.
Overview
Objectives
Our objective was to explore daily self-reported experience of axial spondyloarthritis (axSpA) flare based on data entered into the Project Nightingale smartphone app, between 5th April 2018 - 1st April 2020.
Methods
In collaboration with data scientist Stanley Ng from the charity White Swan, we used machine learning (a type of artificial intelligence) to cluster participants based on symptom scores during self-reported flare. Only participants with 10 or more days of data entry were included for the machine learning analysis. Baseline characteristics and mean flare on versus flare off values were reported for each identified cluster. Differences between clusters were assessed using a statistical method called Welch’s t-test.
Results
189 participants had data available between 5th April 2018 - 1st April 2020. 143/189 (75.7%) participants recorded at least 1 flare. Each flare lasted an average of 4.30 days (range 1–78 days), with an average frequency of once every 35.32 days (range 1-677 days). Significant relationships were identified between flare status and variable scores. Two clusters of participants were identified with distinct flare profiles.
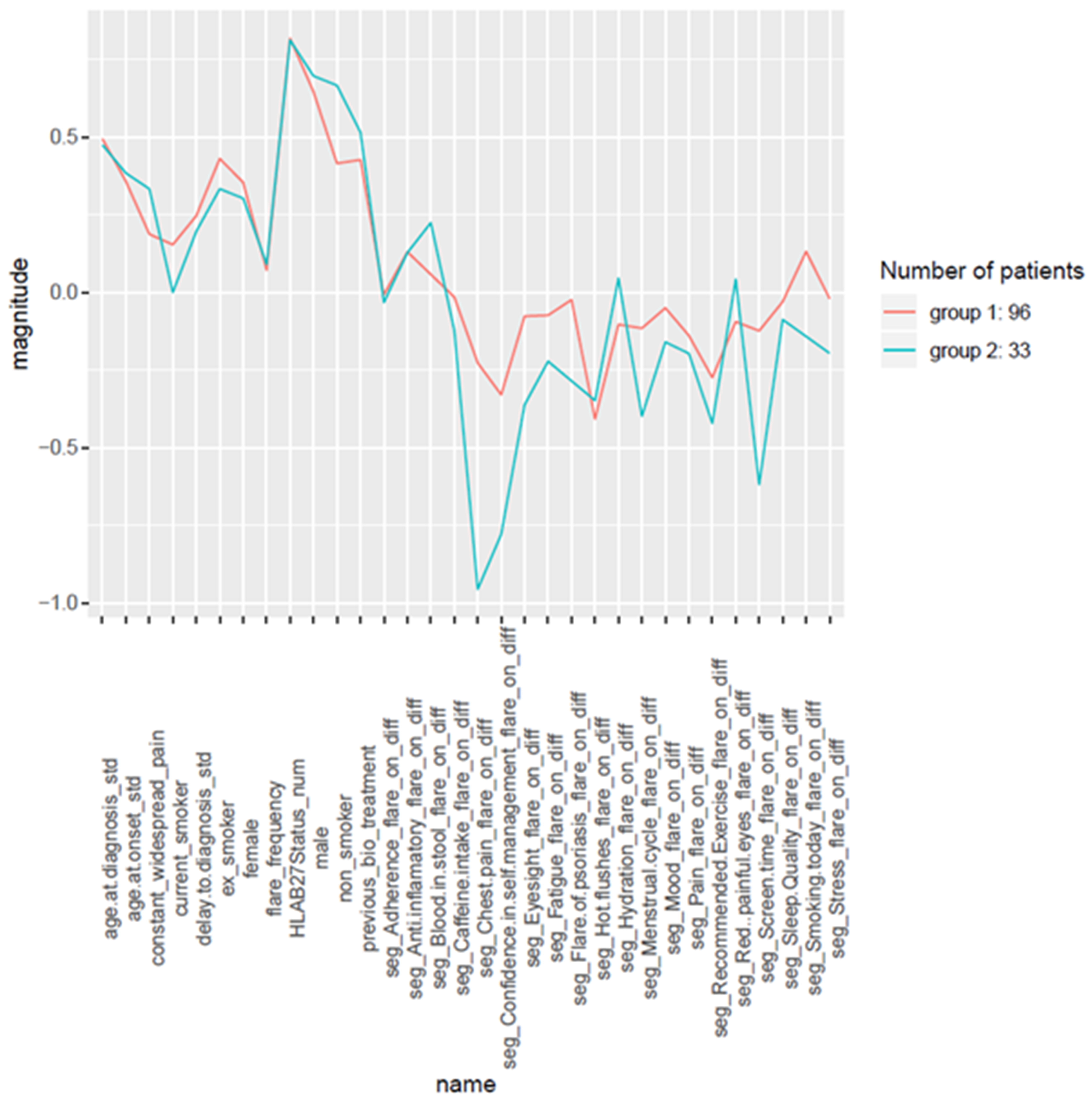
Group 1 experienced less severe worsening of symptoms (pain, fatigue, sleep, mood and stress) during flare in comparison to Group 2. However, they experienced significantly longer flare duration (7.2 versus 3.5 days); perhaps indicating a prolonged, yet less intense flare experience. Groups were similar in terms of flare frequency and clinical characteristics. You can see the differences in smartphone scores vs clinical characteristics between the two groups in the figure below (differences “normalised” to between -1 and 1).
Conclusions
Two clusters of participants were identified with distinct flare experiences, but similar baseline clinical characteristics (e.g. disease activity, spinal mobility, function). Highlighting the potential of smartphone technologies to capture subtle, potentially critical changes in disease activity that are not currently considered in clinical practice. Future integration of daily self-reported health data into the electronic health record may allow for greater optimisation and personalisation of treatment outcomes, through more accurate reporting of disease experience. Innovative, data driven tools should be explored in clinical consultations, to see if they can improve care for people with axSpA. Furthermore, the study of such daily self-report data may in future allow for prediction of flare based on patterns of symptoms/behaviour or enable a greater understanding of behaviours that lead to earlier resolution of flare. This may facilitate earlier targeting and prevention of flares to reduce flare frequency and duration – to ultimately improve quality of life for people with axSpA.
About the journal
Rheumatology Advances in Practice, an official journal of the British Society for Rheumatology, provides a global forum for the publication of the highest quality clinical papers on all areas of rheumatology and musculoskeletal practice, in a fully open access, online journal environment. The journal is an essential resource on therapy, imaging, education, qualitative research, health economics, rare rheumatic diseases, and translational science.