7th Bath, Bristol and Weston Combined Axial Spondyloarthropathy Meeting
Hi all!
You may be interested to hear that last week was the 7th Bath, Bristol and Weston Combined Axial Spondyloarthropathy Meeting; this time hosted and chaired by Dr Raj Sengupta. This educational meeting is held regularly for healthcare professionals of the Bath, Bristol and Weston area, to share and discuss research and treatments, to optimise care for people with axial spondyloarthritis (axSpA).
We felt privileged to present a talk discussing Project Nightingale, and our aim to improve the assessment of axSpA through remote monitoring of symptoms, in order to provide a better overall picture of the condition and the impact it has day to day. We discussed ongoing research at the University of Bath, including the work of William Hue and Dr Simon Jones; exploring the integration of self-tracking data into healthcare, and designing tools to best use self-tracking data to support patient-clinician conversations and personalise and optimise treatment plans. We shared some of our initial research results also, including those presented in previous blog posts. Thank you again to all of you for being a part of Project Nightingale, and for all of your efforts thus far!
In addition to the correlation analyses data, we also presented some information on demographics and engagement – some of which we think you may be interested to see below!
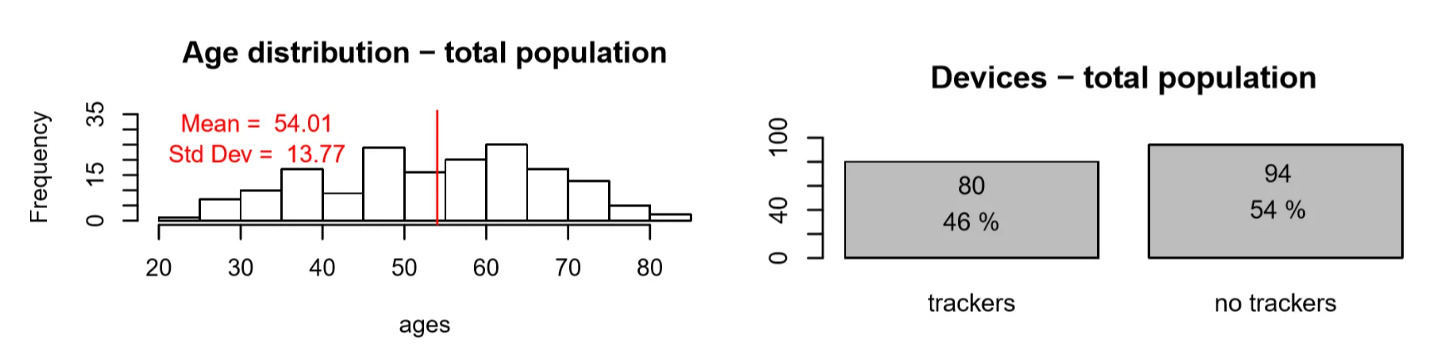
The following graphs utilised data extracted from Project Nightingale on 8th March 2019. At this time, 174 of you had consented to research. As you can see, the age distribution of users spreads from the ages of 20, all the way up to the over 80s! While approximately half of users registered at this time appeared to be using wearable activity trackers.
There was a range of 1-323 days of data logged over the total period; with users logging an average of 99.7 days of data – a huge amount of data!
The meeting itself was fascinating – with lots of discussion and interest in our work. There were also brilliant talks by Dr Raj Sengupta, discussing the move towards personalised medicine in axSpA, incorporating discussions on both disease assessments and treatments. Raj discussed many topics, including the iPad project at the Royal National Hospital for Rheumatic Diseases. As many of you may be aware, the iPad project has allowed for questionnaire data that you fill in before your clinic appointment to automatically be uploaded to the axSpA hospital database. This allows your Rheumatologist to view your data graphically during your appointment and track your condition over time; observing aspects such as spinal mobility, disease activity, quality of life and fatigue. Not only this, but the amazing database team at the hospital have ensured that they have been through every individual’s paper notes and uploaded all historical measures into the database also. So that your clinician can see changes in your condition since your very first appointment!
Later in the afternoon, we had a talk from Romy Schwäbe; Doctoral student at the University of Bath and qualified physiotherapist for over 15 years. Romy is an experienced, hands-on, passionate musculoskeletal physiotherapist, currently studying part-time for a Professional Doctorate in Health, while owning a Sports Physiotherapy centre near Bath. Romy discussed the current field of axSpA physiotherapy research and standard practice in both the UK and abroad, before outlining her current work towards a doctoral degree, which comprises of scientifically testing physiotherapy methods for axSpA and exercises that are not currently incorporated into standard care. She has currently developed a protocol for this work and is in the process of applying for approvals to begin these studies. Her work is incredibly exciting, and we hope it will have great impact in future in the world of axSpA management.
Dr Peter Rouse from the University of Bath, Department for Health also gave a fascinating talk discussing considerations and ways that we can potentially support people with axSpA when recommending physical activity or exercise. He presented some of his previous work; including discussion of responses from an open survey exploring physical activity experiences in axSpA, whereby the full scientific article can be found here https://academic.oup.com/rheumap/article/3/2/rkz016/5523856. Importantly, Peter’s work has highlighted that people with axSpA can and do participate in a diverse range of physical activities. Participants identified 21 different ways that exercise improved or worsened their arthritis; with 15 of these relating to improvement in symptoms. In particular, respondents highlighted that physical activity keeps their joints mobile (16%), reduces stiffness (14%) and enhances psychological and mental wellbeing (10%).
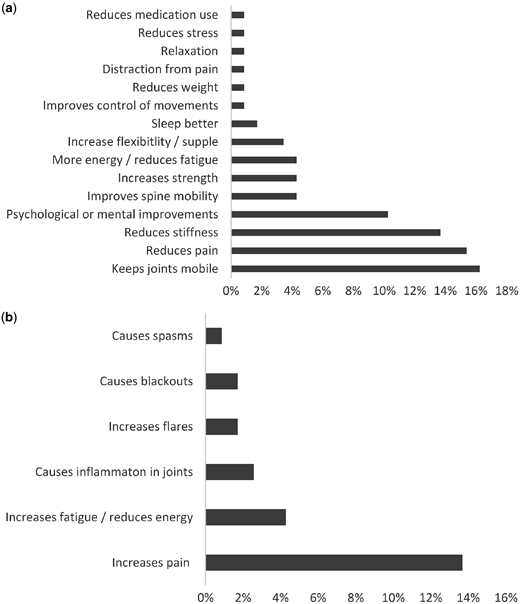
(a) Ways that physical activity improves axSpA symptoms and the percentage of participants who identified each factor. (b) Ways that physical activity worsens axSpA symptoms and the percentage of participants who identified each factor.
‘I feel better when I exercise, my hips are less stiff and I sleep better at night.’
‘Improves my stamina, smoothness of movement, eases any pain.’
Pain relief was identified as a way that physical activity improved symptoms (15%), but at the same time 14% of participants suggested that physical activity can increase pain.
Although reported less, other ways in which physical activity made symptoms worse included increased fatigue or reductions in energy (3%), causing inflammation in joints (2%), causing blackouts (1%) and increases in flares (1%).
‘It worsens me because I never know when to stop, resulting in grossly over doing the activity.’
The over-riding theme, however, was that physical activity can both worsen and improve arthritis symptoms. In total, 34% of respondents highlighted that an optimal level of physical activity was needed to ensure that physical activity had a positive rather than negative impact on their arthritis.
‘I feel as though I can move more freely after the exercise and it does improve, however, on occasions I suffer terribly the next day for days afterwards and have not energy to get out of bed in the morning.’
A wide range of factors (35 in total) that encouraged participation in physical activity were identified by those who were physically active on a regular basis. These included knowing the benefits of participating in regular physical activity (12%), having the support of friends and family (11%), belonging to a support group (9%), reductions in pain (9%) and enjoying the activity (6%). A total of 86% of physically active respondents indicated that their level of physical activity fluctuated from one day to another. Of the 21 different causes of fluctuations identified, fatigue (30%), pain (18%) and work (9%) were the three most frequently cited factors. Other causes of fluctuations in physical activity were the weather, stiffness, family commitments and sedentary behaviour.
The non-physically active participants (n = 32) identified 12 factors that encouraged them to participate in physical activity, including support from a knowledgeable person (13%), wanting to spend time with children (10%) and knowledge of benefits (10%). However, these non-physically active participants most frequently reported that ‘nothing’ encouraged them to be physically active (19%).
To summarise, this study highlighted that self-monitoring and body awareness appear to be crucial when understanding the optimal amount of physical activity to improve arthritis symptoms and not exacerbate them. In addition to confirming that exercise plans should be individually tailored, to optimise levels of physical activity and maximise the benefits for people living with axSpA.
Peter also discussed some recent research by Thomas Ingram; studying toward a Professional Doctorate in Health. Thomas is trying to understand how we can better support people with axSpA to partake in physical activity, following participation in the 2-week axSpA course at the Royal National Hospital for Rheumatic Diseases in Bath.
The afternoon closed with a talk from Dr Katharine Howells, Consultant in Pain Medicine at the Royal United Hospitals Bath NHS Foundation Trust. She discussed some of the implications of chronic pain, and again, ways to best support people with axSpA who experience chronic pain; through providing tools to help manage these symptoms and take control of them.
It was a brilliant, informative afternoon with lots of discussion and interest. We hope you find some of the above information useful also.
Thank you for reading – have a fantastic weekend!