2022 – A year in axSpA research! Part two
Hello Everyone!
I hope everyone is keeping safe in this stormy weather.
Today’s blog continues with research updates for 2022. Below are a few articles from February 2022. The topics include 1) satisfaction with switching from Humira (adalimumab) to a biosimilar, 2) enthesitis in axial spondyloarthritis, and 3) sleep apnoea in ankylosing spondylitis.
Influence of information provided prior to switching from Humira to biosimilar adalimumab on UK patients’ satisfaction: a cross-sectional survey by patient organisations
February 2022. Kaneko and colleagues. https://bmjopen.bmj.com/content/12/2/e050949
In 2018, Humira’s patent expired (the patent of the originator adalimumab drug) and biosimilars could be produced (officially approved versions of originator drugs which cost much less). NHS Trusts and clinical commissioning groups received guidance that at least 80% of people already taking Humira should be switched to or remain on the “best value” biologic within 12 months.
This switching may cause anxiety and even suspicion as people think the main reason for changing to a “best value” drug is to save costs. However, switching can mean lots of things including successfully creating value across the whole health and social care system – not just assessing the comparative cost of drugs. There is a lot of complex clinical evidence required to prove that the biosimilar and originator are therapeutically equivalent prior to approval of a biosimilar. The below video was developed by the Patients Association and provides an overview of what biosimilars are, in addition to explaining why some of these switches have happened.
The satisfaction and perceptions of people who have already switched to a biosimilar from Humira is unclear, therefore the aim of this study was to investigate the perceptions and experiences of the process of switching from Humira to biosimilar adalimumab. A survey was completed by 899 people with immune mediated inflammatory diseases for which biologic tumour necrosis factor inhibitors (TNFi) may be prescribed. People included in the survey were identified after having made contact with various patient organisations including The National Rheumatoid Arthritis Society (NRAS), National Axial Spondyloarthritis Society (NASS), Crohn’s & Colitis UK (CCUK) or Psoriasis Association UK. The type of conditions included were rheumatoid arthritis (RA) /juvenile idiopathic arthritis (25%), axial spondyloarthritis and ankylosing spondylitis (AS; 19%), skin psoriasis and psoriatic arthritis (PsA; 13%), Crohn’s disease (CD; 42%) and other inflammatory bowel diseases such as ulcerative colitis (UC; 1%). Most of the participants (52%) in the survey had been taking Humira for 1-5 years; 62% were ‘very well controlled’ in disease activity prior to switch, and 26% ‘well controlled’.
Key findings:
· Forty-three per cent of people who took part in the survey raised concerns about switching with the healthcare team, but 16% did not have their concerns satisfactorily dealt with.
· Over half of respondents (53%) reported not being asked for consent before switching.
· Only 8% were ‘very satisfied’ with their biosimilar adalimumab after the switch, while 34% were ‘not at all satisfied’.
· More than half reported that they were not given an option to decline the switch or to delay it (56% and 52%, respectively).
· After switching, the most commonly reported problem was that of ‘worse pain’ on injection with the biosimilar compared with originator. The injection pain was said to be ‘much worse’ by 51% and ‘slightly worse’ by 23%.
· Regarding symptom control, 47% reported it to be the 'same' or 'better than' with originator. However, 20% reported that their symptoms were ‘much worse’.
· Those with higher disease activity tended to report greater dissatisfaction with all aspects of the switching process.
· Those who were ‘dissatisfied’ with the written and verbal communication from their healthcare providers had worse perceptions of the switch process, such as worse side effects, pain when injecting, the ease of using the injection device, and managing symptoms.
· People who were ‘satisfied’ with the training for the new injection device reported fewer side effects, less pain when injecting, and reduced difficulty in use of the injection device after the switching process.
The findings of the survey revealed that the level of communication provided when switching to a biosimilar was not adequate, and that dissatisfaction with provided information was associated with more negative perceptions of switching to the biosimilar. After having switched, problems were reported such as worse pain on injecting and worse symptom control, and those with higher disease activity were dissatisfied with the entire switching process. This highlights the importance of providing clear, co-produced information about the switch to a biosimilar as well as appropriate training in the use of a new injection device.
If you have a story about switching to a different drug that you would like to share, feel free to email me on: ns2271@bath.ac.uk
Enthesitis in patients with psoriatic arthritis and axial spondyloarthritis- data from the Danish nationwide DANBIO registry
February 2022. Mathew and colleagues. https://www.sciencedirect.com/science/article/pii/S0049017221002286?via%3Dihub
Enthesitis is inflammation at the entheses- the attachment sites of tendons, ligaments, or joint capsules to the bones. It can be a common symptom in people with spondyloarthritis, such as psoriatic arthritis (PsA) and peripheral spondyloarthritis. In axial spondyloarthritis (axSpA), enthesitis has been reported to be present in around 21-56% of people. Clinical enthesitis is defined as tenderness, with or without swelling, at the entheses.
DANBIO is a Danish clinical registry where people with various medical conditions are monitored as part of routine care.
The aim of this study was to explore the frequency and relation to disease activity of enthesitis in PsA and axSpA in the nationwide Danish DANBIO registry. In this registry, information on core clinical disease activity measures, patient-reported outcomes (PROs) and treatment are collected. Registering the assessment of enthesitis in the registry was possible from 2010 onwards, therefore the data for this study focuses on 2010-2020.
For those who were first registered in DANBIO between 2010 and 2020 (incident cohort - 6,582 people with PsA and 5,547 with axSpA) these were the key findings:
· Enthesitis was not frequently assessed.
· There was no data on enthesitis for 5,545 (84%) of the PsA group, and 4,359 (79%) of the axSpA group.
· A total of 2,225 people had record of entheseal assessment at their first visit, of whom 39% with axspA had enthesitis and 66% with PsA had enthesitis.
· Women more frequently had enthesitis than men in both PsA (61% vs 39%) and axSpA (62% vs 37%).
· The proportion of axSpA people with positive HLA-B27 was lower in the enthesitis group as compared to the non-enthesitis group (54% vs 69%).
· Spinal mobility measured by BASMI was worse in those who had enthesitis.
· People with enthesitis had higher disease activity, worse PROs and fewer had patient acceptable symptom state, emphasising the importance of this clinical domain in SpA
This study showed that enthesitis was common among those who had assessment of entheses between the years 2010-2020. However, enthesitis was assessed only in a minority of visits which indicates a need for an increased focus on systematic enthesitis assessment among rheumatologists. This is particularly important as people with enthesitis had higher disease activity in this study.
Have you experienced enthesitis, and how was this assessed by your rheumatologist? If you would like to share your story, feel free to email me on: ns2271@bath.ac.uk
Prevalence and factors related to sleep apnoea in ankylosing spondylitis
February 2022. Wiginder and colleagues. https://link.springer.com/article/10.1007/s10067-021-05924-z
Obstructive sleep apnoea (OSA) is a condition with episodes of upper airway collapse, resulting in periods of apnoea (absence of breathing for short periods) and hypopnoea (slower breathing than normal) during sleep. Studies have suggested there is a link between ankylosing spondylitis (AS- the radiographic form of axial spondyloarthritis) and OSA, with around 8.8% of people with AS suffering with OSA compared to 5.1% in the general population. Not enough is known about OSA in AS therefore this study was conducted to:
1) Investigate how common OSA is,
2) Explore the sleeping patterns in people with AS compared to the general population,
3) Determine factors associated with OSA in people with AS.
One hundred and fifty-five people with AS were included in the study, and 2,500 people from the general population in Sweden (known as the control group). All participants were given a home sleep-monitoring device (ApneaLink Air®, ResMed, CA, USA) to use for one night. The device was able to monitor various patterns of apnoea and hypopnoea, which could be classified as mild, moderate or severe. However, this home monitoring-device does not replicate a diagnosis of sleep apnoea or sleeping disorders. Participants completed the Epworth sleepiness scale (ESS) which measured the risk of falling asleep during the day.
Comparison between people with AS and matched controls
Forty-six people with AS were matched with up to four people from the control group (a total of 179 people) based on age, sex, weight, and height. Of the 46 people with AS, 47.8% had OSA: 18 (39.1%) had mild, four (8.7%) had moderate, with none severe. Of the control group, 50.8% (91/179) had OSA: 69 (38.5%) had mild, 17 (9.5%) had moderate, and five (2.8%) had severe OSA.
OSA in people with AS
· Sixty-three people with AS fully-completed the home sleep-monitoring (see Table 1 for participant characteristics).
· Of these 63 participants, 25 (39.7%) people had OSA and 38 (60.3%) people didn’t have OSA.
· Twenty people (31.7%) had mild OSA, five (7.9%) moderate, and none were severe.
• People with AS and OSA were older and had higher BMI than people without OSA.
• People with AS and OSA had lesser chest expansion versus people without OSA.
Table 1. Participant characteristics in 63 people with AS 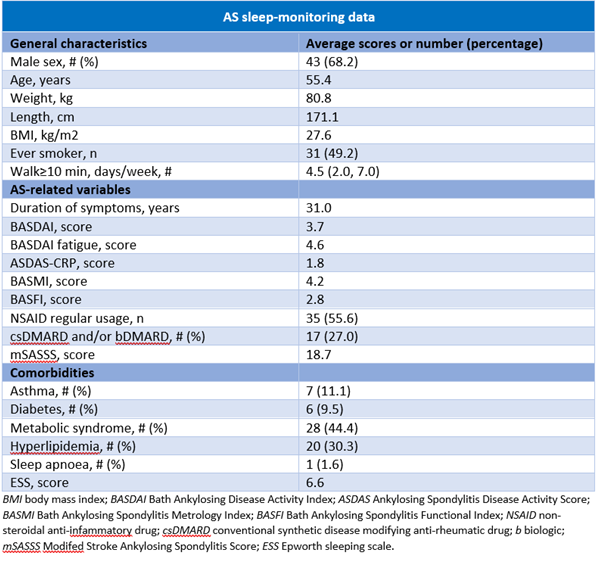
This study found no difference in the proportion of OSA between people with AS and people from the general population (control group). However, it is important to remember that a home-monitoring device was used and not a polysomnography, so this does not provide a confirmed diagnosis of sleep apnoea or sleeping disorders. In people with AS, being older age and having higher BMI were associated with OSA.
Have you been diagnosed with obstructive sleep apnoea, and have ankylosing spondylitis? Feel free to share your experiences of the condition. You can email me at: ns2271@bath.ac.uk
Summary & Sign Off!
I hope you have enjoyed reading these summaries of research, and found the information useful.
If you want to share your experience of any issues related to this blog, please contact me on: ns2271@bath.ac.uk. I would love to hear from you!
Best Wishes,
The Project Nightingale Team