2021 – A year in axSpA research! Part one
Hello Everyone!
I hope all of our readers are well, and continuing to keep safe.
Today’s blog is the latest in the publication updates, and we have made it to 2021! For those who are new to the Project Nightingale blogs, or may not be aware, we are currently posting 3-month article summaries from previously published research on axial spondyloarthritis (axSpA). This blog post is for articles published from January to March 2021.
Happy reading!!
Physiotherapists' awareness, knowledge and confidence in screening and referral of suspected axial spondyloarthritis: A survey of UK clinical practice
January 2021. Steen and colleagues. https://onlinelibrary.wiley.com/doi/10.1002/msc.1537
This article begins by presenting some of the information we have previously seen in other articles on the delay to diagnosis and reasons for this delay. One of the key reasons for the delay has been identified as the lack of awareness of, and screening for, axSpA. The authors state that awareness and knowledge of axSpA has been explored amongst General Practitioners and other medical specialities, however, there has not been research carried out to date into awareness of, and confidence of, musculoskeletal physiotherapists in assessment and referral of possible axSpA. As musculoskeletal specialists frequently assess people with back pain, they have a key role to play in identifying and referring suspected axSpA and improving delay to diagnosis. As such, this research study aimed to 1. assess physiotherapists' clinical reasoning and management decisions on people presenting with persistent back pain, 2. examine their ability to differentiate inflammatory back pain and axSpA from other back pain, and 3. evaluate awareness of National Institute for Health and Care Excellence (NICE) guidance on back pain and recognition of clinical features and referral criteria for suspected axSpA.
Physiotherapists who had at least one experience of treating persistent back pain were asked to complete a survey including examples of clinical presentations of symptoms, based on real patient cases. For each case presentation, respondents were asked to give their diagnoses, their ‘clinical reasoning’, direction of ‘further subjective screening’ and the management strategy.
- Only 60% of respondents (79 out of 132) were able to correctly identify a case of axSpA.
- Ninety‐four percent of respondents (50 out of 53) incorrectly diagnosed axSpA as non‐specific back pain.
- Not surprisingly, those with accurate answers were more familiar with NICE guidance on spondyloarthritis and had continuing professional development (CPD) on spondyloarthritis, and had higher professional grade.
- Non-recognition of axSpA was associated with less than 3 years musculoskeletal experience.
- Only 4% of respondents who correctly identified axSpA mentioned the NICE guidance baseline (i.e. starting point) referral criteria in their ‘clinical reasoning’.
Of the 79 physiotherapists that correctly identified the axSpA cases, encouragingly 92% made an appropriate management decision of referral for specialist opinion. Sixty one percent of these were referred to rheumatology.
Correctly identifying axSpA was associated with higher confidence levels (8/10) in knowledge of clinical features of inflammatory back pain, the extra‐ articular and peripheral features associated with spondyloarthritis. However, confidence was still high in many respondents (59%) who inaccurately diagnosed axSpA. When asked about the knowledge of features of inflammatory back pain (a key axSpA feature), only 27% of respondents recognised all features of inflammatory back pain (9/9), and only 44% identified all additional NICE referral criteria (4/4).
The survey found limited awareness, knowledge and confidence in the recognitions of features of inflammatory back pain, associated extra‐articular conditions and other features that are associated with suspicion of spondyloarthritis. Physiotherapists are commonly involved in the assessment and screening of persistent back pain, and some concerns have been raised regarding their role in appropriate and timely referral for specialist assessment. Therefore, physiotherapists are an important target for raising awareness of axSpA and professional education on recognition and referral to improve this issue. The misattribution may be partly due to poor awareness of the clinical features of axSpA, along with how common non‐specific back pain is (90%–95% of people reporting back pain).
One finding in this study was key: better recognition and appropriate referral were associated with physiotherapists' familiarity with NICE (2017) guidance on spondyloarthritis and previous professional education on spondyloarthritis. This suggests that educational campaigns to raise awareness of axSpA NICE guidance may improve recognition and referral of axSpA. This research study was published before the actonaxialspa campaign (https://www.projectnightingale.org/blogs/good-morning/; https://www.actonaxialspa.com/) was launched to raise the profile of axSpA among healthcare professionals such as physiotherapists, and it shows the huge impact that raising awareness can have. With the actonaxialspa campaign now launched, we can hope for improved recognition and referral of suspected axSpA once physiotherapists and other healthcare professionals have been trained and educated.
Ovarian reserve in patients with ankylosing spondylitis
January 2021. Bahat and colleagues 2021. https://link.springer.com/article/10.1007%2Fs00404-020-05824-8
SpA is the second-most frequent rheumatic chronic inflammatory disease, particularly in women of child-bearing age. However, little is known about the impact of the disease and its treatments on fertility. The aim of this study was therefore to investigate the autoimmune effects of ankylosing spondylitis (AS), or radiographic axSpA (r-axSpA), on the fertility potential of women with AS/r-axSpA by evaluating their ovarian reserves. This was done by checking antral follicle count (AFC), serum anti-Müllerian hormone (AMH) levels and basal follicle-stimulating hormone (FSH) levels. Serum AMH level is an indicator of the follicle pool, and is commonly used to monitor ovarian reserve in patients who are at a higher risk for infertility.
Fifty-two women with r-axSpA, regular menstrual cycles (21–35 days), with cycle length variations of less than 4 days, with both ovaries intact, non-smokers, who had no history of serious illnesses (such as liver failure, malignant diseases, chronic renal failure), infertility or other gynaecological conditions (such as abnormal uterine bleeding), and who had not been on hormonal or herbal medication during the previous three months were included in the study. Another group of 52 healthy women were included in the study as a ‘control’ group, to allow for comparison of results. The results of the comparison showed that the average ovarian volumes for both right and left ovaries were similar in both groups. However, the average serum AMH levels were a lot lower in the r-axSpA study group when compared to the control group, and the average AFC was also a lot lower in this group. The average FSH levels did not show any differences in the study group and the control group.
Some studies suggest that serum AMH levels are lower in women of reproductive age with autoimmune disorders. However, this is the first study to investigate the serum AMH levels and AFC in women with axSpA. The low levels of serum AMH and AFC observed in the AS/r-axSpA group of this study were interpreted as a reduction in the ovarian reserves of AS/r-axSpA women compared to healthy women. The authors conclude that women with AS/r-axSpA positive mothers or siblings should be advised accordingly in terms of the risk factors on their fertility potential, as the chances of premature ovarian failure or early menopause may be possible. However, it is important to note that there is very little literature on infertility in axSpA, and a need for more robust studies to understand fertility in axSpA before drawing such conclusions. Furthermore, this study only included 52 women which is not representative of the AS/r-axSpA population and we therefore cannot draw any firm conclusions. It is, however, great to know that such important research is being done into fertility in axSpA. Indeed, a recent systematic review on fertility and pregnancy found only 2 prior studies on fertility in axSpA (both self-report questionnaire studies showing no evidence of increased infertility risk) – highlighting the need for further, robust studies on fertility in axSpA.
Please visit the National Axial Spondyloarthritis Society (NASS) Facebook page for more information on this topic, and also reach out for help if you have been affected by topics related to infertility. NASS suggest that the single most important piece of advice about planning a family when diagnosed with axSpA is to discuss it with your rheumatology team in advance.
Driving difficulties in patients with axial spondyloarthritis: Results from the Scotland Registry for Ankylosing Spondylitis
March 2021. Morton and colleagues. https://doi.org/10.1002/acr.24595
Driving is a common choice of transport, and particularly for those with reduced mobility driving is often the only option to retain independent mobility. Having to give up driving has, consequently, been found to be associated with social isolation, restricted mobility, and depression. Very little is known about how axSpA impacts driving ability. People who are diagnosed with axSpA are very often of working age, and as we know, driving is important for participating in work. Recently it has been identified that commuting to/from work can be a particular issue. The authors set out to investigate how common driving difficulties are in people with axSpA, the nature of those difficulties, their association with factors such as demographic information and clinical features of the disease, and the impact of driving difficulties on work ability in axSpA.
The Scotland Registry for Ankylosing Spondylitis (SIRAS) is a disease register of patients with a diagnosis of axSpA in Scotland. People from this registry were included in a study where clinical data were collated, and socio-economic/lifestyle characteristics were collected by postal questionnaires. There were two parts to the study: the first part included all individuals who had indicated in the first questionnaire that they currently drove a motor-vehicle; the second part included current drivers who were also in paid employment. From the clinical data collated, participants were labelled as high or low disease activity; three categories of pain: chronic widespread pain (CWP), widespread pain (not chronic), or regional pain; fatigue, and anxiety/ depression were also recorded. Driving difficulties were measured by a list of nine tasks (see Table 1) that people had to score from 0 (no difficulty) to 3 (severe difficulty). Other factors measured were access to an urban area and work productivity, i.e. whether individuals had missed any work due to their axSpA in the past seven days, as well impairment while working.
Table 1. Tasks included in driving difficulties and number of people (percentage) affected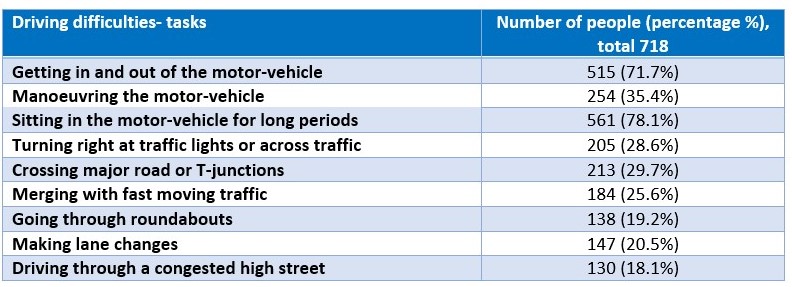
Of the 718 current drivers, 642 (89%) had some difficulty with at least one driving task and 72 (10%) had some difficulty with all nine tasks. Getting in/out of a car and sitting for long periods were the most frequently reported difficulties.
Three common groups, or domains, were created from the nine driving tasks. These were dynamic driving scenarios (Domain 1), crossing traffic (Domain 2), physical act (and comfort) of driving (Domain 3). Below are some findings from the study related to the domains:
1. People with higher disease activity; regional, widespread, or chronic widespread pain; knee pain; lower back pain; mid-upper spinal pain; and moderate-severe fatigue were more likely to have difficulties with all three driving difficulty domains.
2. People who had retired early or who were unemployed due to their health were more likely to have difficulties with all three driving difficulty domains when compared with employed individuals.
3. People in paid employment who had predominantly physical/labour intensive jobs were more likely than those who had sedentary jobs to have driving difficulties, in particular, with the physical act of driving.
4. People who had only completed secondary school or further college education were also more likely to have difficulty with the physical act of driving relative to those who had completed a university degree.
5. Each of the identified driving difficulty domains was associated with a greater likelihood of work-related presenteeism and absenteeism.
This study raises awareness of driving difficulties in axSpA. It has enabled the concept of driving disability to be further refined and identified which aspects of driving cause difficulties for people with axSpA. The three domains are consistent with the types of adaptations people with musculoskeletal conditions report making in order to keep driving (such as making detours to avoid certain routes that involve crossing traffic or dynamic driving situations, and choosing a car to improve the physical act and comfort of driving).
Driving difficulties are common in people with axSpA and are adversely associated with work participation. Improving understanding and awareness of driving disability in axSpA will ensure the right advice and resources are made available to enable people to remain independent and economically active.
Has your driving ability been affected by axSpA? What affects did this have on your lifestyle? Feel free to get in touch and share your stories: ns2271@bath.ac.uk
Please also visit the National Axial Spondyloarthritis Society (NASS) Facebook video which shows you some tips related to driving from osteopath Zoë Clark (who has axSpA), such as how to get in and out of the car safely, positioning yourself in the car to maximise comfort, and choosing the right type of car for you, amongst other things.
Summary & Sign Off!
I hope you have enjoyed reading these summaries of research.
If you have been affected by any of the information in these summaries, please reach out to help and support available here.
If you want to share your experience of any issues related to this blog, please contact me on: ns2271@bath.ac.uk. I would love to hear from you!
Best Wishes,
The Project Nightingale Team